Published: 25/11/21 13:20 Categories: Microbiology
The current pandemic has drawn attention to urgent public health issues. One of the most important issues, which could be the next global challenge, is the loss of effectiveness of drugs for treating infections, that is, antimicrobial resistance.
What does antimicrobial resistance mean?
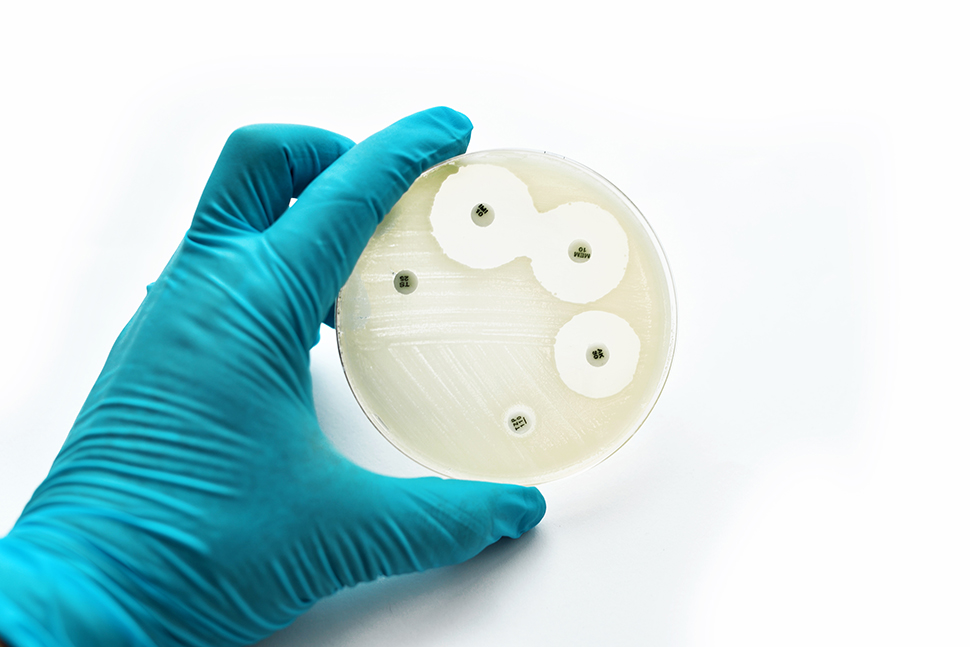
A common misconception is that it is the body that becomes resistant to microorganisms, which is wrong, as antimicrobial resistance (AR) occurs when microorganisms such as fungi or bacteria develop the ability to 'defeat' substances designed to eliminate them, which means that the pathogens continue infecting the organism and, yet more worrying, developing.
The difficulty of this resistance lies in the fact these infections are very complicated and often impossible to treat. Every year in the U.S. alone, 2.8 million people and 670,000 in the E.U. suffer from an antibiotic-resistant infection, and deaths are estimated at 35,000 and 33,000 respectively.
This issue has the potential to affect anyone, regardless of age or health condition, although it is true that people with chronic diseases are at especial risk. AR is also relevant in sensitive situations such as organ transplants, oncological therapies and chronic disease treatments.
Why does AR occur?
Due to the ubiquity of microorganisms, some of which are harmless and others pathogenic, their resistance strategies are of concern, which include restricting access to, directly eliminating, changing, destroying, avoiding or even modifying the targets of antimicrobial substances.
And the fact is that any antibiotic can give rise to resistance, as these traits can be inherited from generation to generation through mobile genetic elements as well as transduction, conjugation and transformation processes.
While it is true that AR occurs naturally due to mutations in the genes of microorganisms, the overuse and inappropriate use of antimicrobials accelerates the spread of resistant pathogens, which is why the Delegated Regulation (EU) 2021/1760 was published in early October with criteria for the designation of antimicrobials with reserved use for human health.

However, this threat is not exclusive to human health, as it also affects veterinary and agricultural industries, since the therapeutic substances used to treat and prevent infections in animals in the food industry belong to the same ones used for humans. This means that animals can also be infected with resistant microorganisms. This is basically the 'One Health' approach, that is, single global human, animal and environmental health.
In addition, certain resistant bacteria such as Campylobacter and Salmonella have been associated with food consumption, as they can be transferred from animals to humans through food. There is also a risk from direct contact with infected animals. However, the main cause lies in the use of antibiotics for human and animal medicine.
If you would like to learn more about the main antimicrobial resistant microorganisms, such as MRSA, Candida, ESBL, VRE and KPC and the products we have available for their analysis, feel free to download our material.

 Food fraud: How do we detect it?
Food fraud: How do we detect it?
 Visit Us at MEDICA 2025 – Discover Our Precise Detection Solutions
Visit Us at MEDICA 2025 – Discover Our Precise Detection Solutions
 PCR: The Technique Revolutionizing Rapid Detection in the Food Industry
PCR: The Technique Revolutionizing Rapid Detection in the Food Industry
 How Culture Media Ensure the Safety, Efficacy, and Quality of Medicines
How Culture Media Ensure the Safety, Efficacy, and Quality of Medicines
 Meeting us at MEDLAB MIDDLE EAST 2025
Meeting us at MEDLAB MIDDLE EAST 2025